What is ICSI?

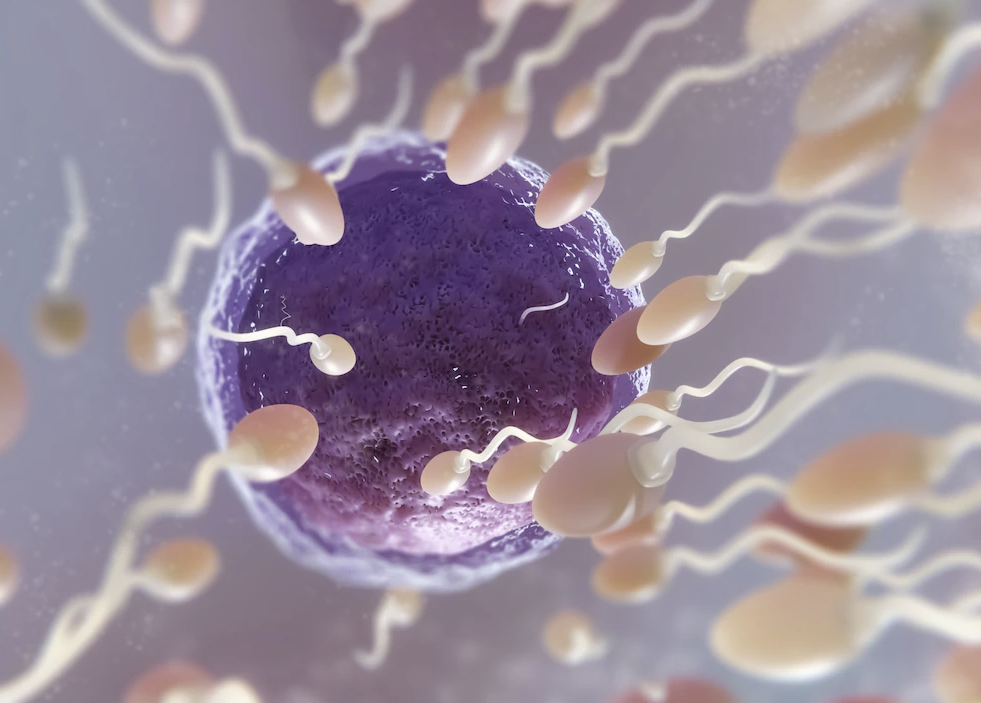
ICSI, commonly known for its abbreviation in English for Intracytoplasmic Sperm Injection, is an assisted reproduction technique that forms part of In Vitro Fertilisation treatment and is used in the majority of fertility clinics.
This technique involves introducing one spermatozoid into the cytoplasm of one of the female’s eggs for the purpose of achieving fertilisation, and later on a pregnancy.
When do we utilise ICSI in assisted reproduction laboratories?
To understand this term you will first need to know what in vitro fertilisation is. In vitro fertilisation (IVF) involves obtaining eggs from the female’s ovaries through a simple procedure called egg retrieval; these eggs will later be inseminated with sperm in the laboratory. The sperm may be from the patient’s partner, or it may be donor sperm in the case of single mothers.
There are two ways insemination can be performed: the first is through conventional IVF which involves putting the spermatozoids in contact with the eggs on a Petri dish in hopes that fertilisation will occur.
The other method is ICSI, a technique that is carried out using intracytoplasmic microinjectors. These microinjectors are microscopes that feature micro-handling equipment that allow the embryologists to microinject, with a microneedle, one single spermatozoid into the cytoplasm of one egg.
Once they have been microinjected, the eggs are left to develop in the incubator and the following day the embryologists will confirm whether fertilisation has taken place.
For what types of patients is ICSI indicated?
The medical specialist is the one who will decide if this technique should be used, and this decision will depend on each patient’s particular case.
In cases for which we use sperm from the partner/spouse:
- Previous failed cycles with artificial insemination.
- Unexplained infertility.
- Absence of or damaged fallopian tubes.
- Endometriosis.
- Low sperm count/poor sperm motility.
- Ovulation abnormalities.
- Immune-related causes.
- Advanced maternal age and the need to perform PGT.
In cases for which we use donor sperm:
- Very severe male factor infertility.
- Previous failed cycles using partner sperm.
- Single females.
- Same-sex female couples.
- Advanced maternal age and the need to perform Pre-Implantation Genetic Testing (PGT).
At any rate, even if a patient meets the requirements for conventional IVF, many fertility clinics prefer to use the ICSI technique to obtain the highest possible fertilisation rates.
Success rates with ICSI:
Generally speaking, fertilisation rates using ICSI are quite high. We can say that between 70-80% of eggs correctly fertilise when the ICSI technique is used, meaning that 7 to 8 eggs fertilise for every 10 that are microinjected.
Between the time of fertilisation and the days of embryo development that follow, not all embryos will be viable or apt for transfer to the female’s uterus. Here you can read more about embryos and their classification before they are transferred to the patient.
There are times when we may observe fertilisation rates that are much lower than the average, or we may even observe something called fertilisation failure which is when no eggs have fertilised.
This article written by our clinic director and senior embryologist, Dr Miguel Lara, will help you better understand fertilisation failure and its possible causes.
It’s very rare for fertilisation failure to occur, but it happens. These cases will require a comprehensive analysis of the patient’s case before proceeding with a new cycle of assisted reproduction treatment. A complete review of the patient’s case is the only way we will be able to draw valid conclusions and determine the best way forward in order to minimise, to the extent possible, the likelihood of obtaining the same outcome again.
Is there a greater risk of congenital malformations when using ICSI?
There are many studies that have been published on this topic, all of which conclude that there is a slightly higher risk of congenital malformations when using ICSI than compared to children conceived through natural conception; these studies, however, conclude that this slight increase can be attributed to the couple’s own cause of infertility.
At any rate, the different scientific societies, including the Spanish Fertility Society, are keeping a close eye on these potential problems.
Preparing the eggs for ICSI
Once the eggs have been retrieved through ovarian puncture, they will remain in the incubator for a few hours so that they can finish maturing.
After about 3-4 hours, the embryologists will be able to begin working with the eggs to prepare them for microinjection.
Preparing the sperm sample for ICSI.
The male will need to provide the laboratory with a sperm sample obtained through masturbation; at the time the sample is provided he should have a sexual abstinence of between two to five days.
It is also very important that no more than 45 minutes has gone by between the time the sample is obtained and the time it is handed in to the assisted reproduction specialists.
The male partner normally provides the sperm sample while the female is undergoing the egg collection procedure. The laboratory can also work with a frozen sperm sample if it’s not going to be possible for the male to provide a fresh sample on the day of egg retrieval; the laboratory can also work with sperm obtained via testicular biopsy in the event that the male has azoospermia or has previously undergone a vasectomy.
Once the sperm sample has been received by the laboratory staff, it will undergo a process called sperm capacitation. Sperm capacitation essentially consists in eliminating seminal plasma from the ejaculate in order to retrieve the spermatozoids with the best motility and the highest fertilisation potential.
Do you have any other questions? Contact us and ask! We’ll be happy to help you!